SFMA - Level 1: Certification
-
Filosofie met focus op patronen en de behoefte voor diagnosticeren
-
Specifiek analyseren van ‘the Big 7 Patterns’ (waar kijken we naar en waarom?)
-
Introductie van het concept van de ‘breakouts’ (hoe analyseren we een disfuncties in bewegingspatronen?)
-
Introductie in interventies (Isoleren/Integreren/Functionele patronen)
-
Een Evidence-Based cursus met ‘state of art’ kennis
Deze cursus is geschikt voor (sport)fysiotherapeuten, manueel therapeuten en chiropractoren.
Wanneer het klinisch onderzoek is geïnitieerd vanuit het perspectief van bewegingspatronen, dan heeft de therapeut de mogelijkheid om belangrijke beperkingen in de keten te analyseren die in eerste instantie geen relatie lijken te hebben met de aanwezige klacht, maar uiteindelijk toch de oorzaak zijn van deze beperking of dysfunctie. Dit concept is beter bekend als ‘regional interdependence’ en is de basis van de SFMA.
Het is van essentieel belang dat therapeuten inzicht hebben in de relatie tussen de verschillende lichaamssegmenten en hoe ook beperkingen in een bepaald segment een negatief effect kunnen hebben op de functie van een segment elders in het systeem. Deze benadering, vanuit het perspectief van bewegen (het SFMA model), maakt het mogelijk om (spier)disbalans en regional interdependence op een logische en methodologische manier te herstellen.
In de SFMA zijn drie concepten van belang. Deze concepten zijn essentieel in relatie tot de progressie van de behandelfases die de patiënt doormaakt en de te selecteren oefeningen en manuele interventies.
Concept 1 - Functioneel continuüm:
- De onbewuste disfunctie
- De bewuste disfunctie
- De bewuste functie
- De onbewuste functie
Concept 2 - De 3 ‘’R’s’’:
- Reset
- Reinforce
- Reloading
Concept 3:
| Four Positions: | Four Types of Resistance: |
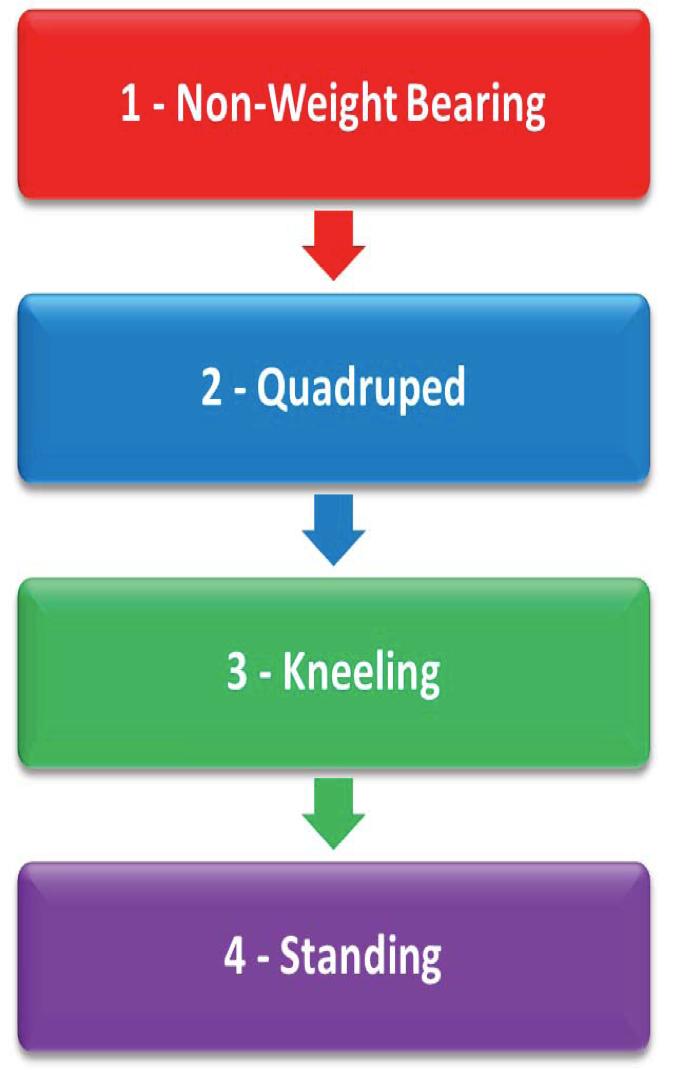 |
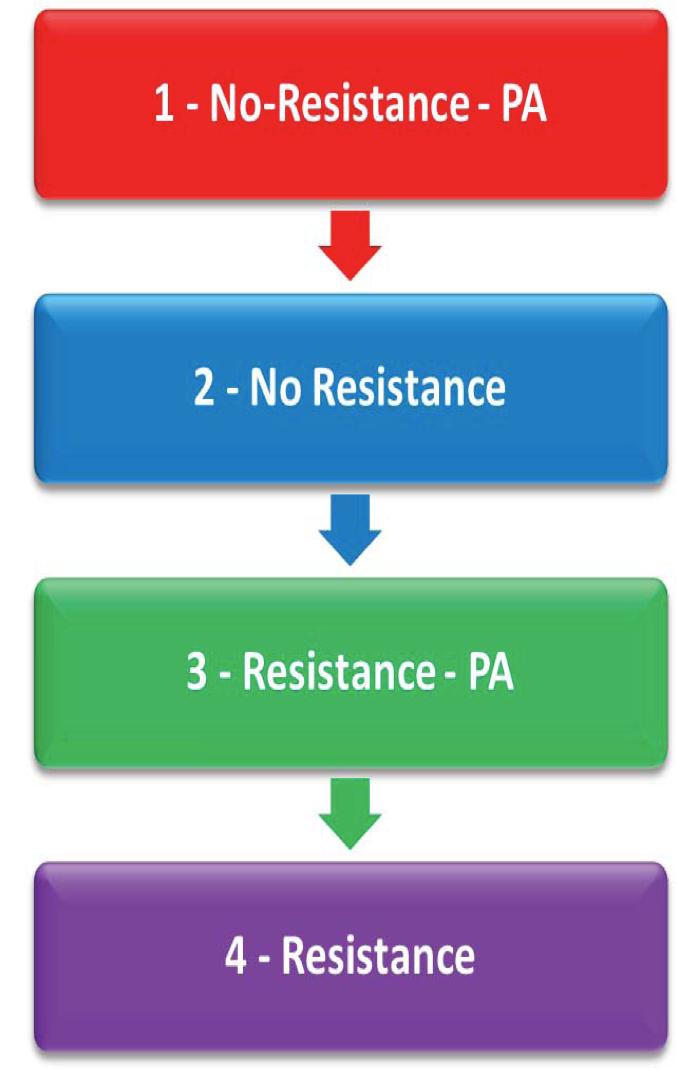 |
Het onderzoek:
Elke testbeweging in de SFMA wordt beoordeeld op:
- Functioneel en niet pijnlijk (FN)
- Disfunctioneel en niet pijnlijk (DN)
- Functioneel en pijnlijk (FP)
- Disfunctioneel en pijnlijk (DP)
Het onderzoek navigeert de therapeut uiteindelijk naar de meest disfunctionele en niet pijnlijke bewegingspatroon, welke vervolgens tot in detail wordt onderzocht. Deze benadering is ontwikkeld om het doorgaans gebruikte standaardonderzoek aan te vullen en dient als model om op efficiënte manier concepten over ‘houding’, spierbalans en de fundamentele patronen van bewegen te integreren binnen het musculoskeletale behandelsysteem.
Bij het herstellen van het meest disfunctionele en niet pijnlijke bewegingspatroon (DN), wordt dit patroon dus niet nadelig beïnvloedt door pijn. Ten eerste moet men proberen om compenserend gedrag te verminderen of te verwijderen en is het belangrijk om de beperkte mobiliteit te verbeteren. Vervolgens geeft men activiteiten en oefeningen die motor control herstellen op een niveau dat in overeenstemming is met de functionele SFMA-status. Dit betekent dat oefeningen moeten worden gebruikt op of onder het functionele niveau van de SFMA break-out test. De flowcharts schrijven voor dat patronen waarbij pijn aanwezig is behandeld moeten worden, maar niet getraind en beweegpatronen waarbij disfunctie is zonder pijn juist wel geoefend moeten worden .
Filosofie:
Normaal bewegen is mogelijk door de integratie van fundamentele bewegingspatronen met een adequate balans van mobiliteit en stabiliteit, afhankelijk en onder invloed van de uit te voeren taak. Veel goed functionerende componenten zijn nodig voor pijnvrij bewegen, zoals een goede houding, ROM, spierkracht, ‘motor control’ en balans. Beperkingen binnen deze componenten kunnen in potentie veranderingen teweegbrengen in functioneel bewegen, die kunnen leiden tot pijn of de beperkingen kunnen juist ontstaan als gevolg van pijn.
Ons bewegingsapparaat laat voorspelbare compensatoire bewegingspatronen zien als respons op pijn of bij de aanwezigheid van zwakte, stijfheid of structuurafwijkingen. Na verloop van tijd zal deze door pijn gedicteerde beweging leiden tot ‘beschermend’ bewegingsgedrag, of zelfs de angst om te bewegen. Dit resulteert uiteindelijk in klinische waarneembare beperkingen, zoals ROM, spierlengte veranderingen en afname in kracht. Een puur lokale benadering voor de evaluatie of behandeling van de klacht zal in veel gevallen niet leiden tot volledig herstel van de functie.
Door middel van theoriepresentaties en veel praktijksessies krijgt de cursist de mogelijkheid om een systeem aan te leren waarbij de uitkomsten van het onderzoek gebruikt worden om uiteindelijk tot een diagnose te komen. Hieruit ontstaat een effectieve behandeling die uitermate geschikt is voor bijvoorbeeld patiënten die niet reageerden op eerdere ondergane behandelingen.
Na het volgen van deze cursus heeft u de volgende kennis opgedaan:
- Het kunnen identificeren van disfunctionele bewegingspatronen
- Pijn veranderingen kan veroorzaken in het bewegingspatroon en ‘motor control’
- Met de uitkomsten van het onderzoek therapeutische oefeningen en interventies voorschrijven of toepassen
- Het belang inzien van het identificeren van de belangrijkste beperkingen die bijdragen aan disfunctioneel bewegen, vanuit neurologisch oogpunt en in relatie tot de regionale en segmentale interactie van betrokken structuren
- Gebruik kunnen maken van de SFMA, FMS en Y-balance test tijden de complete functionele evaluatie van een patiënt
- Het kunnen analyseren van veranderingen in disfuncties en beperkingen om het trainingsprogramma te aan te kunnen passen
- Kunnen beschrijven waarom het belangrijk is om bewegingspatronen te onderzoeken in zowel belaste als onbelaste posities en hoe u vervolgens deze informatie kunt gebruiken in de interventies
-
Het kunnen ontwikkelen van Evidenced-Based revalidatieprogramma’s voor specifieke pathologieën die zijn gebaseerd op huidige wetenschappelijke research
Er staan geen cursussen gepland. Vul uw gegevens in om op de hoogte te blijven van nieuwe cursussen.